You want to be there for others but find yourself holding back – whether that’s because you don’t know what to say or how to say it, or you’re worried you’ll make the problem worse.
For many of us, offering support to someone struggling isn’t easy – and often does not come naturally. Whether that’s a family member, friend or a colleague, we often want to help, but don’t know how to.
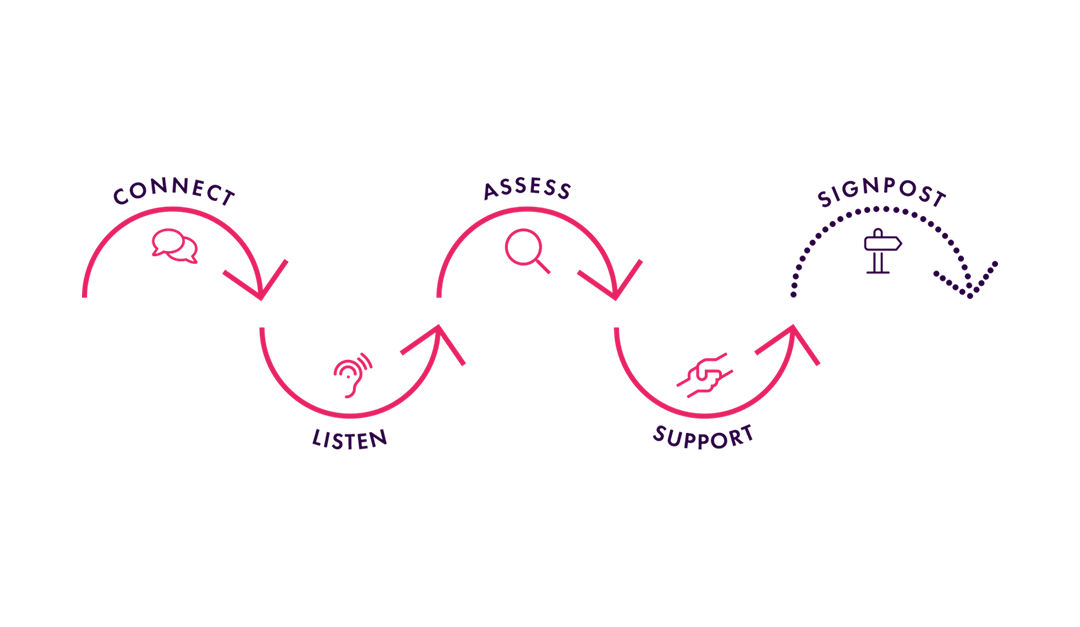
That’s why we created a simple five-step process to give you the skills to support the mental health of others: The CLASS Approach.
Mental health is something that fluctuates and can depend on all sorts of factors – from the actions you take to the thoughts you have. Everybody can have good days, bad days and those average days in between.
And because everybody has mental health, we all have a role to play in supporting those around us; including those people you consider to be the ‘strongest’, or those you’d never think would struggle.
It’s crucial that we’re comfortable and confident in having these conversations and can support others when they need it most. That’s why the CLASS Approach is so important.
Note: If you believe your friend, colleague or family member has reached a point of crisis, read our guide on supporting others in crisis.
How do you know when to offer support?
Before we guide you through the CLASS Approach, you may be wondering: “How do I know when to offer support?”
When it comes to spotting someone struggling, there can be hundreds of warning signs and these hints can be as unique as the person is. Sometimes there might not be any warning signs at all.
That’s because those who struggle with their mental health can become experts at masking how they’re feeling, putting on a brave face to convince people that they’re managing okay.
Instead, we should be checking in with how someone is feeling whenever we can – whether we think they’re struggling or thriving.
But there is another approach to take: if something doesn’t feel quite right, it often isn’t.
It may be that the person is more distracted in conversation, preoccupied with their thoughts or acting a bit out of character.
Maybe they’re turning down social invitations or turning up a bit late to work. Perhaps they seem a bit flatter in mood than usual. No matter how small or subtle the difference, it’s definitely worth checking in and seeing how they’re doing.
The CLASS Approach
The CLASS Approach will give you the confidence to connect, listen to, assess, support and signpost the person you’re talking to so they can get the right help at the right time.
1. Connect
The first thing to do is to connect with the individual. For many of us this can be the most challenging part.
When something doesn’t feel quite right, connect with the person you’re concerned about by starting a conversation with them. You could say:
“Hey John, you don’t quite seem yourself today, how’s everything at home?”
Or: “Hi Lindsey, I’ve noticed you’ve not been your usual self lately, is there anything you’d like to chat through?”
Starting a conversation gives them the opportunity to open up.
In some situations, everything might genuinely be okay. In others, they may be struggling and might not want to talk about it.
And that’s fine – you can’t force them to speak about anything they don’t want to. But, what you have done is ‘left the door open’ for them, so they can come back to you if they want to in the future.
Alternatively, you may find that the person you’re concerned about approaches you directly, or perhaps indirectly by making ‘off the cuff’ comments like “I’m feeling a touch off”, “I’m fed up with everything” or “I’ve had it up to here”.
This will give you an opportunity to ask open-ended questions to see how they’re feeling. For example: “What is it in particular that you’ve had enough of?”
2. Listen
Once you’ve made that connection, it’s vital you listen with empathy and show compassion.
As humans, our instinctive response to hearing a problem is to find a solution – but when it comes to mental health, this is something we should refrain from doing.
It’s not our role to ‘fix’ or solve the person’s problem. Instead, we should make them feel heard, listened to and understood.
There are two key skills when it comes to doing this: verbal listening and non-verbal listening.
Verbal listening skills refer to tuning in to what’s being said, and reflecting this back periodically to check your understanding.
For example, try using phrases like “What I’m hearing is…” or “It sounds like…” and then summarise what they’ve just said.
This will help the person know you’re understanding and processing what they’re saying. Remember not to lead or push your own agenda onto the conversation; your role is to facilitate the conversation and listen non-judgementally.
Practice non-verbal listening too, which is conveyed through our body language. Ways of doing this include maintaining steady eye contact throughout and avoiding defensive body language, like folded arms.
3. Assess
While you’re listening, it’s important to assess the situation and consider what support the person could benefit from.
You’re not expected to be a mental health professional, so it’s not your responsibility to know exactly how to help them.
Instead, you’re there to support them with finding the right help. You also shouldn’t create a plan of action on their behalf – this must be a collaborative effort between the two of you.
Questions to ask when assessing include:
- Have you been struggling for a while or is this just a bad day?
- Are you seeing a mental health professional?
- Are you experiencing thoughts of suicide or self-harm?
If any of these questions raise concerns, it’s important to find a collaborative way forward, and signpost to the relevant services (which we’ll discuss shortly).
If someone does express suicidal thoughts, there are additional factors to think about and actions to take. To learn about these, read our guide on suicide prevention.
4. Support
For someone struggling, knowing that you are there to support them can make all the difference. In fact, a strong support network is often cited as one of the most helpful ways to get through a mentally challenging period.
Provide support during this initial conversation. Here, it’s important that you’re empathetic, meaning that you should try to see things from their perspective, and reassure them that you’re there to help and they’re not a burden to you.
Continue to support that person after the conversation too. Keeping this dialogue open is one of the most important things, as it means they can come back to you if they are still struggling.
5. Signpost
The vast majority of us are not GPs, therapists or counsellors – so you’re not expected to have all of the answers.
Because of this, it’s important to signpost on to other specialist services when an individual is struggling, so they can get the support they need.
There are different types of support available, and it can be overwhelming to know which service is best. But a good place to start is encouraging them to see their GP, who will be able to carry out a basic mental health assessment and refer them onto specialist support if necessary.
If they’re not sure about seeing their GP, they could instead self-refer to the NHS therapies service, or contact one of the many mental health helplines available, such as:
It’s also important that you don’t break confidentiality – unless you are concerned for the safety of the person you are supporting.
The CLASS Approach: Takeaways
Everybody has mental health, and it’s important we feel confident and comfortable to check in with our friends, family and colleagues.
Be brave, connect with the other person and open up the conversation. It could be the lifeline they were waiting for.